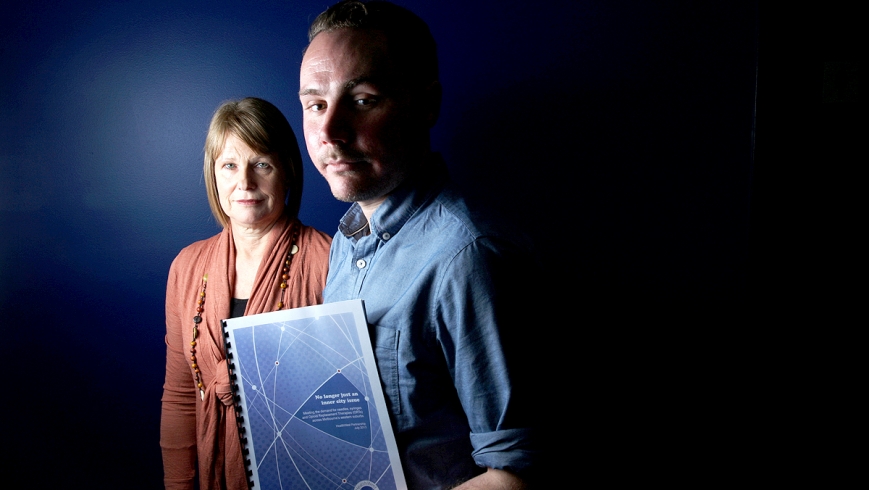
SHORTAGES of clean syringe programs and GPs prescribing methadone will lead to more drug-related deaths in Melbourne’s outer west, warns a report revealing the heroin scourge is “no longer just an inner-city issue”.
Demand for injecting equipment in the outer west has increased faster than anywhere else in Melbourne, with Health Department figures used in the report showing syringe distribution has more than doubled in a decade, far exceeding population growth of 40 per cent.
While Maribyrnong has the most injecting drug users in the west, the report by care network HealthWest reveals the problem is worsening in outer areas.
Demand for needles and syringes in Brimbank increased 211 per cent, to more than 306,000, from 2002-12. Wyndham recorded a rise of 173 per cent, to 199,500 last year.
Demand for methadone, a heroin replacement dispensed from pharmacies, increased 390 per cent in Melton and by 165 per cent in Wyndham in the same period.
More than 460 people across Melton and Wyndham are on methadone, placing a heavy burden on the four local GPs who are actively prescribing it.
HealthWest project manager James Dunne said the lack of drug safety programs in outer suburbs meant “the cycle of drug addiction keeps going”.
“People are having to travel quite far to access GPs who prescribe methadone, but methadone distributors aren’t located evenly across the west – they’re clustered around commercial centres,” he said.
“Because large patches are going without pharmacies, that seriously affects a person’s ability to stay on the methadone program.”
Werribee pharmacist Greg Meaghan, who dispenses methadone to about 85 people a day, said the shortage of prescribing GPs in Wyndham meant patients were at risk of reverting to heroin if they missed an appointment or had a falling out with their doctor.
Mr Meaghan said many doctors were reluctant to prescribe methadone because drug addicts could be aggressive.
Drug addicts in outer suburbs also faced barriers to accessing clean syringes such as the cost of catching public transport to needle distributors in Footscray.
Harm Reduction Victoria executive officer Jenny Kelsall said the consequences of inadequate methadone and syringe programs included more overdoses and HIV and hepatitis C infections.
The HealthWest report urges the state government to establish a safe-injecting facility in the western suburbs, provide greater investment in syringe distribution and methadone programs, actively encourage GPs to prescribe methadone and set up formal links between local health services.
Community Services Minister Mary Wooldridge is reviewing the state’s methadone network and has announced $11 million of funds to open ‘withdrawal beds’ to wean addicts off high doses of methadone and provide extra training to increase providers.